COVID-19 and the skin
– Treatment discontinuation and rate of disease transmission in psoriasis patients receiving biologic therapy during the COVID-19 pandemic: A Canadian multicenter retrospective study
– COVID‐19 cutaneous manifestations: simplifying the confusion
– Oral manifestations of COVID‐19 disease: A review article
– Skin manifestations of COVID-19: A worldwide review
Treatment discontinuation and rate of disease transmission in psoriasis patients receiving biologic therapy during the COVID-19 pandemic: A Canadian multicenter retrospective study.
JR Georgakopoulos, A Mufti, R Vender, J Yeung
Research Letter J AM ACAD DERMATOL VOLUME 83, NUMBER 4
Reviewed by Dr Pan Jiun Yit, National Skin Centre Singapore
“A multicenter retrospective study was undertaken of all patients from 2 tertiary academic hospitals affiliated with the University of Toronto, Canada, and a community practice in Hamilton, Canada. Inclusion criteria were patients aged 18 years or older with moderate to severe psoriasis who received at least 1 dose of a biologic before February 1, 2020. Data were retrospectively obtained from Patient Support Program case managers of all major suppliers of biologic agents for psoriasis. February 1, 2020, was the starting point of data collection (5 documented COVID-19 cases and 0 deaths in Canada) and patients were followed up until June 1, 2020 (91,703 cumulative cases and 7594 deaths).
As of February 1, 2020, there were 2095 patients receiving biologic therapy for psoriasis who met inclusion criteria. Total number of patients who temporarily discontinued their biologic at any point during the 4-month period because of COVID-19–related concerns was 23 (1.1%). Of the 23 patients who temporarily discontinued their biologic, 7 did so in February, 11 in March, 3 in April, and 2 in May. This corresponded to a total of 17 (0.81%), 18 (0.86%), and 18 (0.86%) patients discontinuing treatment at each of April 1, May 1, and June 1, 2020 timepoints, respectively. Biologic discontinuation by class included tumor necrosis factor α inhibitors (8/749, 1.07%), interleukin 12 and 23 inhibitors (5/371, 1.35%), interleukin 17 inhibitors (4/482, 0.83%), and interleukin 23 inhibitors (6/493, 1.22%). Mean duration of biologic treatment before discontinuation was 50.6 ± 35.7 months. Five patients who temporarily discontinued their biologic elected to restart the same biologic before June 1 compared with 18 who remained without treatment. All patients who restarted their biologic (5/5, 100%) did so because of a flare of their psoriasis. Of the 23 patients who temporarily discontinued treatment, 14 (60.9%) were men, mean age was 56.4 ± 12.6 years, and 1 (4.3%) also had psoriatic arthritis. Of the 2095 patients in our cohort (2072 [98.9%] of whom continued to receive a biologic throughout the entire follow-up period), 0 had a confirmed positive diagnosis of COVID-19. All patients who developed COVID-19–related symptoms received testing, results of which were negative. Of the 16 new biologic treatment initiations between April 1 and June 1, 2020, the majority were interleukin 17 inhibitors (n = 13, 81.2%), followed by tumor necrosis factor α inhibitors (n = 2, 12.5%) and interleukin 23 inhibitors (n = 1, 6.2%).
The results of this study demonstrate that the rate of patient-driven biologic discontinuation during the peak of COVID-19 cases in Canada remained low during the entire 4-month follow-up period. Although interleukin 17 inhibitors had the lowest rate of temporary discontinuation, there did not appear to be a major class-specific difference in rates. Discontinuation of treatment out of concerns about contracting COVID-19 is not supported because it may lead to decreased efficacy outcomes with reintroduction or a flare of psoriasis, as observed with our cohort. Low volumes of new biologic initiations highlight the need for improved access to nonurgent care during the pandemic.”
COVID-19 cutaneous manifestations: simplifying the confusion
el‐Azhary, Rokea A., ed. Int J Dermatol. 2021;60(1):3-4
Reviewed by Dr Sean Leong, National Skin Centre Singapore
Covid-19 has affected more than a 100 million patients worldwide. As the number of cases grew, there have been many reports about the myriad dermatoses associated with Covid-19 dermatoses. With an estimated prevalence of Covid-19 related dermatoses ranging from 0.2% in China(1) to 20.4% in Italy(2), it is imperative for us as dermatologists to determine if a patient’s dermatosis is related to the underlying Covid-19 infection.
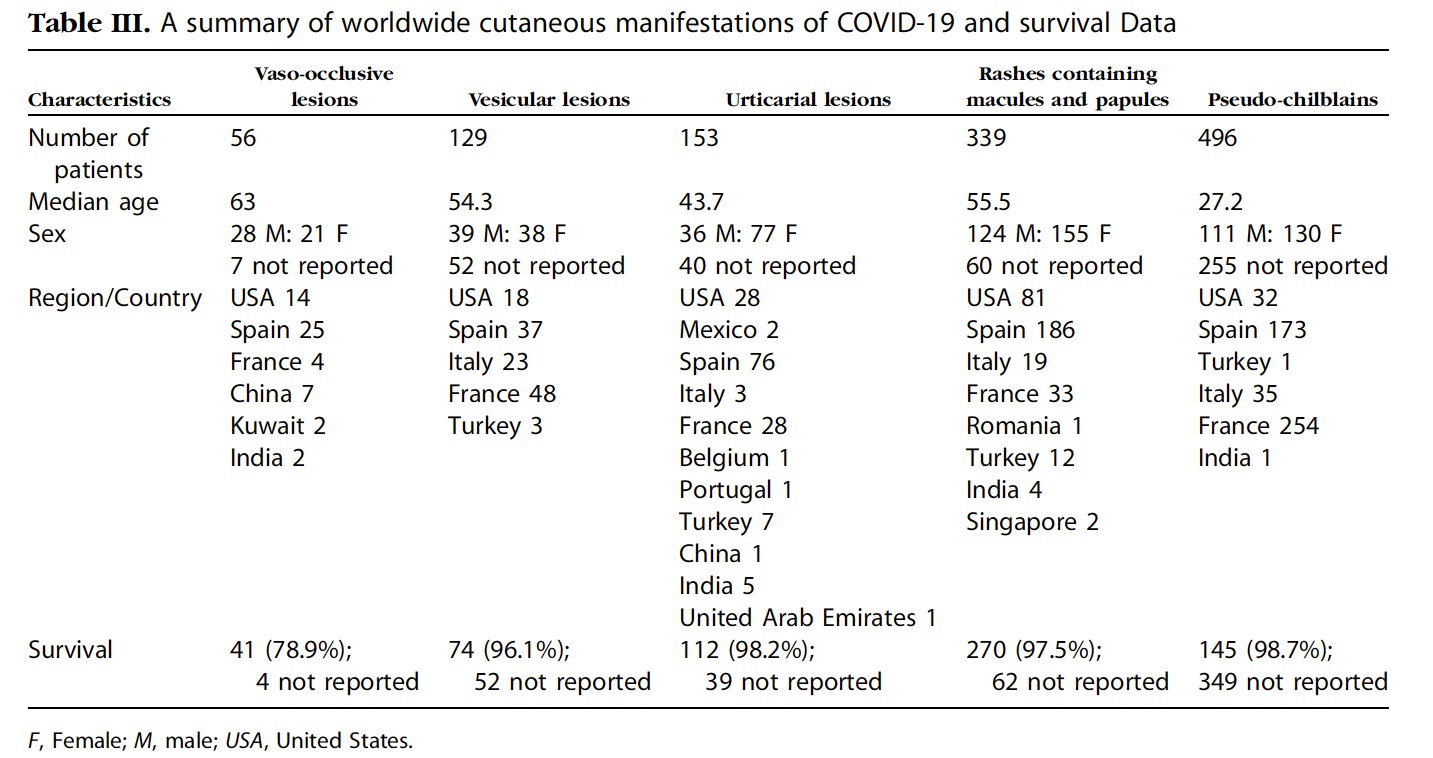
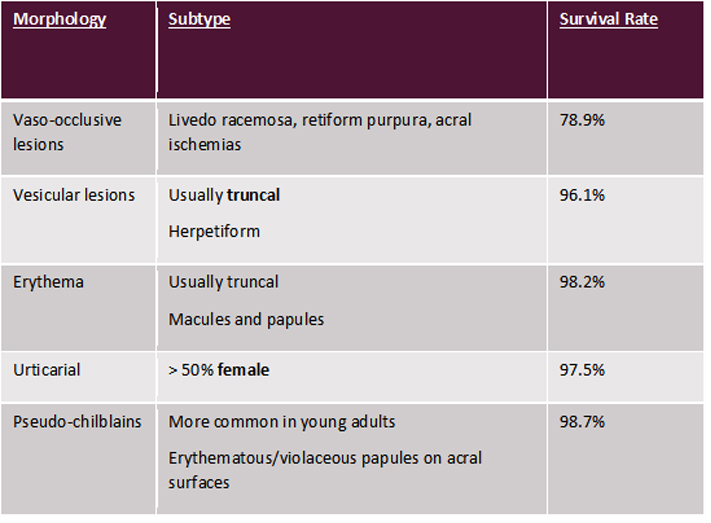
Though the presentations can be varied, a recent systematic review performed by Tan SW et al demonstrated that they can be divided into 5 main categories – vaso-occlusive lesions, vesicular lesions, erythema, urticarial and pseudo-chilblains lesions (see Table 1)(3). Each of these various morphologies has been associated with variable survival rates, with vaso-occlusive lesions being associated with higher mortality in patients.
Table 1: Classification of Covid-19 Dermatoses by Tan SW et a
Histologically, patients with vaso-occlusive lesions demonstrate the presence of microthrombosis in the blood vessels. Previous studies have also demonstrated the presence of heavy deposits of C5b-C9 complements with co-localisation of SARS-CoV2 spike glycoprotein, further supporting the pathogenesis of the virus in the prothrombotic process(4). Other histological presentations of Covid-19 dermatoses include the presence of a coat-sleeve-like lymphoplasmacytic infiltrate around vessels and periadnexal structures(5).
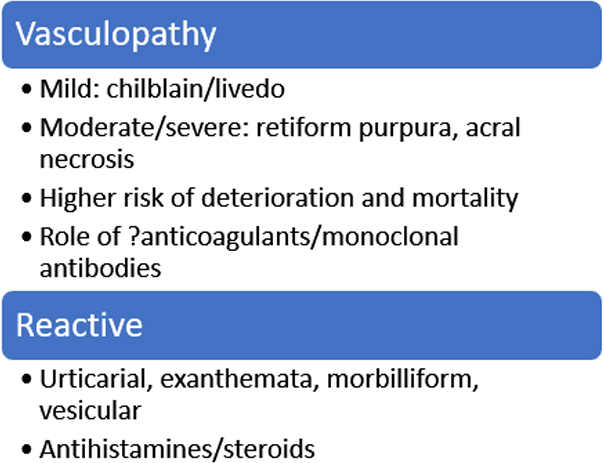
Given the wide gamut of presentations, Dr el-Azhary proposes a simpler classification which is perhaps more useful for the practicing dermatologist (see Table 2). Patients who demonstrate evidence of vasculopathy are at increased risk of developing thrombosis in other systemic organs and it is perhaps incumbent on us to highlight this potential deterioration in patients to the primary physician. Given the pathophysiology, it remains to be seen if the use of anticoagulants or specific monoclonal antibodies against specific complements in the prothrombotic pathway show any efficacy in the treatment of such disorders.
Table 2: Proposed classification of dermatoses by Dr el-Azhary
Dermatologists play an important role in accurately diagnosing dermatoses during this pandemic, especially when some cases may be asymptomatic at the time of cutaneous presentation. With this proposed dichotomy, it may better help us take care of our patients and help guide clinical management in a multidisciplinary setting.
References
1. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708-20.
2. Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34(5):e212-e3.
3. Tan SW, Tam YC, Oh CC. Skin manifestations of COVID-19: A worldwide review. JAAD Int. 2021;2:119-33.
4. Magro C, Mulvey JJ, Berlin D, Nuovo G, Salvatore S, Harp J, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Transl Res. 2020;220:1-13.
5. Ho WYB, Wang D, Tan LYC, Bundele MM, Tan CH, Lim HLJ. Two cases of cutaneous eruptions due to CoVID-19 infection in Singapore: new insights into the spectrum of clinical presentation and histopathology. J Eur Acad Dermatol Venereol. 2020;34(10):e576-e9.
Oral manifestations of COVID‐19 disease: A review article
B Iranmanesh, M Khalili, R Amiri, H Zartab and M Aflatoonian
Dermatologic Therapy. 2021 Jan;34(1):e14578. doi: 10.1111/dth.14578. Epub 2020 Dec 13.
Reviewed by Dr Chia Hui Yi, National Skin Centre Singapore
This review article aims to describe the oral manifestations seen in patients with COVID-19 disease. The authors searched published literature in Pubmed library and Google Scholar and thirty-five articles published in English from December 2019 until September 2020 were selected. Clinical presentations included ulcers, erosions, bullae, vesicles, pustules, fissured or depapillated tongue, macules, papules, plaques, pigmentation, halitosis, whitish areas, hemorrhagic crusts, necrosis, petechiae, swelling, erythema, and spontaneous bleeding. The oral lesions were symptomatic (painful, burning sensation or pruritus) in most cases (68%) and occurred in nearly equal proportions in both genders (49% female, 51% male). The common sites of involvement were the tongue, labial mucosa, palate, gingiva, buccal mucosa, oropharynx and tonsil.
The suggested diagnoses were aphthous stomatitis, herpetiform lesions, candidiasis, vasculitis, Kawasaki‐like, erythema multiforme‐like, mucositis, drug eruption, necrotizing periodontal disease, angina bullosa‐like, angular cheilitis, atypical Sweet syndrome, and Melkerson‐Rosenthal syndrome. The latency period between appearance of systemic symptoms and oral lesions was between 4 days before and up to 12 weeks after the onset of systemic symptoms.
Therapies prescribed were dependent on the aetiology ascribed. The lack of oral hygiene, opportunistic infections, stress, immunosuppression, vasculitis, and hyper‐inflammatory response secondary to COVID‐19 were thought to be the most important predisposing factors.
This study gives a broad overview of the myriad of oral presentations seen in patients with COVID-19 disease, although the pathophysiology behind of the oral lesions remains to be elucidated. While the number of patients included in each category is small and the oral manifestations do not appear to be specific for COVID-19 disease, this study serves to remind clinicians of the importance of examination of the oral cavity and its potential impact on the patients’ quality of life.
Skin manifestations of COVID-19: A worldwide review
SW Tan, YC Tam, CC Oh. Skin manifestations of COVID-19: A worldwide review, JAAD International, Volume 2, 2021, 119-133
Reviewed by Dr Choon Chiat OH, Singapore General Hospital
This article was a systematic review of articles describing cutaneous symptoms associated with COVID-19 infection around the world. The authors searched all related published articles via PubMed, OVID, EMBASE, MEDLINE, and Google Scholar for original and review articles written in English and published from November 11,2019, to September 30, 2020. They summarized the findings of 51 articles in this review, of which 27 were case series and 24 were case reports. A total of 1211 patients were described in these articles.
The authors identified 5 skin lesions common in patients with COVID-19: pseudo-chilblains, rashes containing macules and papules, and urticarial, vesicular, and vaso-occlusive lesions. These lesions manifested at various times in relation to the COVID-19 symptoms, which may indicate whether the lesions are virus-induced or are delayed immunological responses to the infection. Of note, patients with vaso-occlusive lesions were more likely than those with pseudo-chilblains to be admitted to the intensive care unit and to die.
There were demographic differences in the prevalence and the morphology of the skin manifestations in COVID-19. Of the 1211 patients with COVID-19 associated skin manifestations, only 39 (3.1%) patients were from Asian populations and 1172 (96.9%) patients were from Europe and the United States. Pseudo-chilblains were the most common COVID-19 related skin manifestations among Europeans and United States residents, but there was only 1 reported case from Asia. A summary of the findings is summarized in Table III of the article (shown below).
The limitations highlighted in this study include: many of the included studies were case reports/ studies with small sample sizes; and not all the included subjects had COVID-19 confirmatory tests because of the limited resources in certain regions. In addition, the difference between the prevalence of cutaneous manifestations in Europeans and United States residents compared with Asians could be attributable to underreporting in Asian countries.
The authors concluded by highlighting that the polymorphous cutaneous manifestations in patients with COVID-19 infection could potentially reflect a full spectrum of viral interactions with the skin, characterized by direct viral action in infected cells, immune system hyperactivity, and hypercoagulability. Future studies with better scientific documentation would help elucidate the pathophysiologic features and the prognostic factors of the cutaneous manifestations in COVID-19.