COVID‐19 cutaneous manifestations: simplifying the confusion
el‐Azhary, Rokea A., ed. Int J Dermatol. 2021;60(1):3-4
Reviewed by Dr Sean Leong, National Skin Centre Singapore
Covid-19 has affected more than a 100 million patients worldwide. As the number of cases grew, there have been many reports about the myriad dermatoses associated with Covid-19 dermatoses. With an estimated prevalence of Covid-19 related dermatoses ranging from 0.2% in China(1) to 20.4% in Italy(2), it is imperative for us as dermatologists to determine if a patient’s dermatosis is related to the underlying Covid-19 infection.
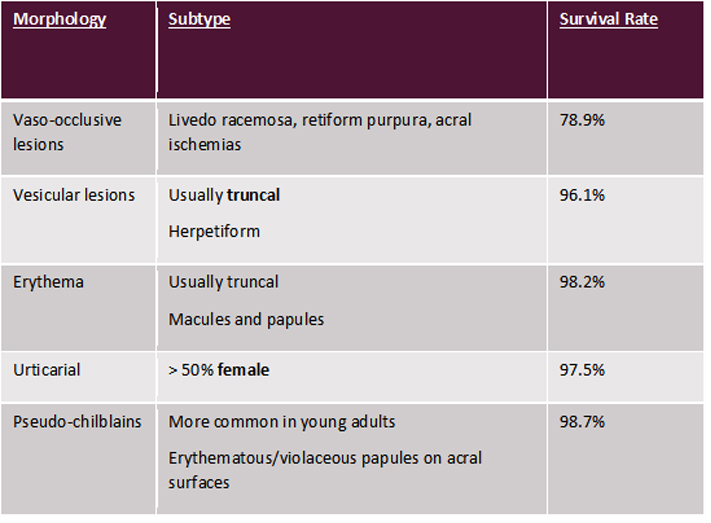
Though the presentations can be varied, a recent systematic review performed by Tan SW et al demonstrated that they can be divided into 5 main categories – vaso-occlusive lesions, vesicular lesions, erythema, urticarial and pseudo-chilblains lesions (see Table 1)(3). Each of these various morphologies has been associated with variable survival rates, with vaso-occlusive lesions being associated with higher mortality in patients.
Table 1: Classification of Covid-19 Dermatoses by Tan SW et al
Histologically, patients with vaso-occlusive lesions demonstrate the presence of microthrombosis in the blood vessels. Previous studies have also demonstrated the presence of heavy deposits of C5b-C9 complements with co-localisation of SARS-CoV2 spike glycoprotein, further supporting the pathogenesis of the virus in the prothrombotic process(4). Other histological presentations of Covid-19 dermatoses include the presence of a coat-sleeve-like lymphoplasmacytic infiltrate around vessels and periadnexal structures(5).
Given the wide gamut of presentations, Dr el-Azhary proposes a simpler classification which is perhaps more useful for the practicing dermatologist (see Table 2). Patients who demonstrate evidence of vasculopathy are at increased risk of developing thrombosis in other systemic organs and it is perhaps incumbent on us to highlight this potential deterioration in patients to the primary physician. Given the pathophysiology, it remains to be seen if the use of anticoagulants or specific monoclonal antibodies against specific complements in the prothrombotic pathway show any efficacy in the treatment of such disorders.
Table 2: Proposed classification of dermatoses by Dr el-Azhary
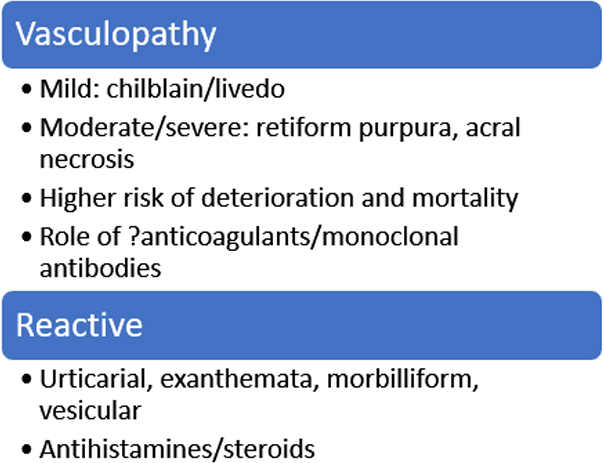
Dermatologists play an important role in accurately diagnosing dermatoses during this pandemic, especially when some cases may be asymptomatic at the time of cutaneous presentation. With this proposed dichotomy, it may better help us take care of our patients and help guide clinical management in a multidisciplinary setting.
References
1. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708-20.
2. Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol. 2020;34(5):e212-e3.
3. Tan SW, Tam YC, Oh CC. Skin manifestations of COVID-19: A worldwide review. JAAD Int. 2021;2:119-33.
4. Magro C, Mulvey JJ, Berlin D, Nuovo G, Salvatore S, Harp J, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Transl Res. 2020;220:1-13.
5. Ho WYB, Wang D, Tan LYC, Bundele MM, Tan CH, Lim HLJ. Two cases of cutaneous eruptions due to CoVID-19 infection in Singapore: new insights into the spectrum of clinical presentation and histopathology. J Eur Acad Dermatol Venereol. 2020;34(10):e576-e9.